A disaster from a Pandemic is different from a Mass Casualty Incident (MCI) where an event results in a number of casualties vastly exceeding local resources and capabilities in a short period of time.
A pandemic follows a bell curve, reaching the peak number of patients halfway through (usually in 5 to 6 weeks), whereas an MCI tapers off quickly. In terms of resource allocation, an ED needs to prepare differently in a Pandemic. This involves an increasing response over a few weeks, keeping in mind that staff and resources may become less available as the situation continues.
A schema for thinking about ramping up to disaster triage and response is illustrated below in Figure 7:
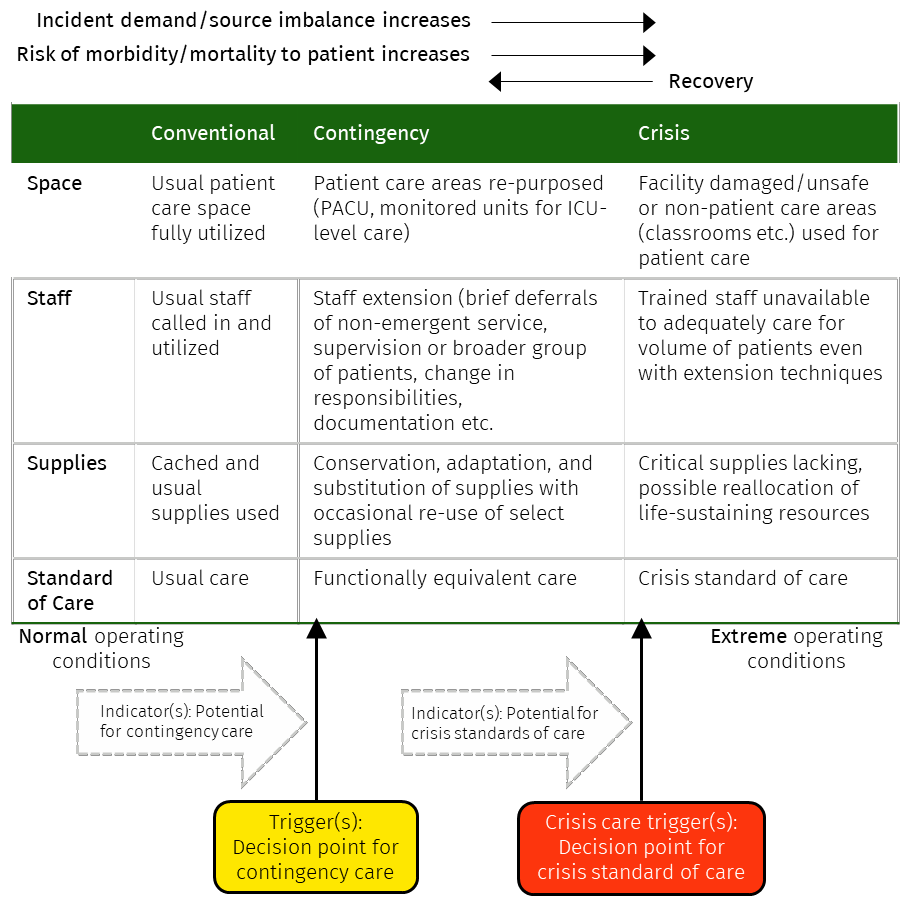
Figure 7. Adapted from: Institute of Medicine. 2013. Crisis Standards of Care: A Toolkit for Indicators and Triggers. Washington, DC: The National Academies Press. https://doi.org/10.17226/18338.[Link]
This requires an ED and whole of health service plan to identify capacity at each stage and trigger points for moving to the next. For example, stages of disaster triage activation may include consideration of:
- Conventional service levels, where a service has suitable space, staff, resources sufficient to deliver usual care;
- Contingency service levels where a service has adapted by enhancing space, staff and resources and engaging with other hospital and community services to enhance capacity.
- Crisis service levels where enhanced resources are overwhelmed and agreed crisis standards of care must be applied. This will necessitate the commencement of Disaster Triage.