This guideline applies to injured patients of all ages.
We recommend that major trauma services retain the capability to perform:
- Acute trauma resuscitation and resuscitative procedures.
- Emergency surgery to preserve life and limb.
We reiterate that there is risk of COVID-19 transmission from:
- Patient to health care worker (HCW).
- HCW to patient.
- HCW to HCW.
We recommend that in any setting, clinicians providing trauma care:
- Consider a patient at high risk for COVID-19 transmission when:
- Patient history or clinical assessment is not reliable or unavailable.
- Clinicians are preparing to deliver trauma care that may include aerosol generating procedures (AGPs), for example pre-hospital or hospital trauma teams receiving trauma patients requiring resuscitation.
- Only consider a patient low risk for COVID-19 transmission when:
- Patient history and clinical assessment has excluded local case definitions.
- No AGPs are required.
- Use senior expertise to limit the number of healthcare workers (HCW) required for safe delivery of trauma care at all stages of the trauma patient journey. This includes and is not limited to:
- Prehospital and inter-hospital trauma care.
- Trauma team activations.
- Transfers to CT, theatre and inter-departmental.
Although the COVID-19 pandemic is likely to reduce traumatic injury presentations overall, there may be a potential skew towards domestic and family violence and self-inflicted injury (Fojut R, ‘How How coronavirus is affecting trauma systems in Italy’. Trauma System News, 21 March 2020. [Link]).
We recommend that:
- Non-accidental injury (NAI), domestic violence, elder abuse and self-inflicted injury are considered in all presentations.
- Emergency clinicians use a domestic violence screening tool (ACEM, P39 Policy on Family and Domestic Violence. [Link]).
We acknowledge and align with:
- The London Major Trauma System: Management of Critical Resources during COVID-19 Pandemic, Clinical Guide for the management of major trauma patients. [Link]
- The American College of Surgeons Committee on Trauma ‘Maintaining Trauma Centre Access and Care during the COVID-19 Pandemic’. [Link]
- The NHS Clinical guide for the management of trauma and orthopaedic patients during the coronavirus pandemic. [Link]
- Australian Orthopaedic Association Position Statement: Orthopaedic surgery during the COVID-19 pandemic. [Link]
- Royal Australasian College of Surgeons Statement: Maintaining front-line trauma services during the COVID-19 response. [Link]
- Australian Orthopaedic Trauma Society: Guidelines for emergency orthopaedic surgery during the COVID-19 pandemic. [Link]
- The NHS Clinical guide for the management of neurotrauma patients during the coronavirus pandemic. [Link]
Exemplar documents:
- Royal Adelaide Hospital: Trauma callouts during COVID era. [Link]
- Gold Coast University Hospital: ED COVID Trauma/Resus Teams Guide. [Link]
-
Early senior consideration of complexity in COVID-19 trauma care

It is well recognised that older patients with injury are at higher risk of delayed diagnosis and poor outcome due to:
- Under-triage in low force mechanism.
- Fewer physiological predictors of severe injury.
- Concurrent cognitive or communication issues complicating assessment.
- Concurrent frailty, comorbidity and polypharmacy.
Older persons are also at higher risk of poor outcome in COVID-19 (see Older Person-Specific section).
We recommend that:
- Trauma teams are led by the most senior trauma clinician available.
- Older injured persons have geriatrician or physician review in line with local guidelines.
- Trauma teams have early discussion regarding patient ceilings of trauma care in line with ethical decision making in COVID-19 (see Ethical Decision-Making section).
- Decisions on limiting trauma care consider the utilisation of critical resources including blood stocks, critical care, emergency surgery and CT scanners.
-
Trauma procedures

In trauma resuscitation, aerosol-generating procedures (AGP) include:
- Airway procedures as listed in the Adult Cardiac Arrest Management section.
- Management of penetrating chest injury.
- Thoracostomy.
- Intercostal catheter insertion (ICC).
- Resuscitative thoracotomy (RT).
We recommend that:
- A robust case by case risk/benefit discussion is conducted prior to commencing any high risk interventions, for example RT, including careful consideration of the predicted outcomes, PPE and other resources such as surgeon availability and usual indications where RT is considered to be of most benefit (cardiac tamponade, signs of life and ongoing cardiac electrical activity).
- Where thoracostomy occurs, ICC insertion should follow as soon as possible to minimise risk of COVID-19 transmission.
- While evidence does not yet exist, ICCs should be connected to low dose wall suction or anti-viral filter to reduce sources of aerosolised particles.
- AGP PPE is used including a face shield and hair cover for all members of the trauma team when AGP is likely to be performed.
Exemplar documents:
- The Royal London T.A.C.T.I.C Resuscitative Thoracotomy in ED (COVID-19). [Link]
- The Royal London T.A.C.T.I.C Chest Drain insertion (COVID-19). [Link]
-
Trauma systems

Multiple new protocols should not be required. We advocate for:
- Senior trauma clinicians to be involved in network and organisational pandemic planning.
- Reviewing existing trauma protocols and guidelines with amendments when required for COVID-19 pandemic. Where patients meet current triage and transfer guidelines for care at major trauma services (MTS):
- Existing guidelines, coordination and referral pathways should be followed where possible.
- Telehealth and senior decision makers at MTS are involved as early as possible.
- Coordinated trauma care communication across state or regional networks, with:
- A centralised communication hub.
- Frequent (as determined by the stage of the pandemic) communication updates at all levels of the trauma network on service capacity including:
- Trauma workforce.
- PPE supply.
- Access to critical resources such as blood stocks, CT and emergency surgery.
- Any impact on standard operating procedures (SOPs) or network guidelines
- Rapid and telehealth supported access for regional and rural services to senior trauma decision makers in MTS.
- Where trauma systems are overwhelmed with unacceptable delays to trauma care, local consideration in consultation with senior trauma clinicians at MTS, for altered trauma care delivery. This may include:
- Consideration of operative intervention where angio intervention is unavailable.
- Consideration of delayed, interventional radiology or non-operative management of injuries.
- In exceptional circumstances, moving trauma HCW to the patient when it is not possible to move the patient. This would allow for use of aeromedical platforms but should be balanced against staff safety and resource capability at both referring hospital and MTS.
- Supporting regional/rural clinicians with appropriate skills to work at an extended scope of practice.
-
Prehospital care

We advocate for:
- All prehospital trauma clinicians to make early assessment of COVID-19 risk.
- All prehospital trauma notifications include information on patient COVID-19 risk based on:
- Ability to assess against local case definitions.
- Requirement for AGPs.
- Objective assessment of potential for escalated care requirements with patient observations, in line with ACEM’s Australasian Triage Scale (ATS) [Link] and local ambulance service guidelines..
We recommend that any pre-notification of COVID-19 suspected or confirmed trauma patients is included in communication to all members of the trauma team response, including and not limited to; the trauma facility lead for COVID-19 clinical care, clinicians, imaging, pathology, administrative, social work and transport staff.
-
Location of trauma care

In the COVID-19 pandemic, trauma providers will need to balance the risks and benefits and timing of patient transfer within the trauma network, with the impact of COVID-19 on:
- The severity of patient disease (injury and non-injury).
- The risk of COVID-19 transmission amongst patients and HCW.
- Trauma system resources and capacity, including:
- PPE availability.
- Workforce distribution across rural/regional and metropolitan trauma services.
- Blood product availability, including stock levels and distribution.
- CT scanners.
- Access to critical care and emergency surgery.
When prioritisation is required, we recommend:
- Only patients meeting pre-hospital major trauma criteria are streamlined to MTS specifically those:
- Requiring ongoing resuscitation.
- Requiring interventional radiology or surgical care.
- Having injuries that require specialised care or intervention such that life, limb or long-term function may be at risk. This may include and is not limited to; solid organ injury of spleen and liver, limb amputation, suspected spinal cord injury, crush injuries, fractured pelvis, open limb fracture or joint dislocation.
- That non-MTS are supported to provide initial patient care and early consultation is required prior to transfer of patients with isolated single system injury without compromise, for example:
- Orthopaedic extremity injuries (excluding pelvic injury).
- Spinal injury without neurological compromise.
- Less than three (3) rib fractures without respiratory compromise.
- Head injury with GCS 14 or 15, including small volume subdural for non-operative management
- That consultation is required prior to any transfer to MTS for patients with the potential for a poor outcome and need for palliative care. These include:
- Patients with advanced care directives that limit the use of critical care and surgical interventions.
- Patients considered very frail and/or vulnerable to adverse outcomes due to advanced age, dementia, and multiple comorbidities, specifically advanced lung disease.
We do not recommend transfer to MTS where adult patients have no evidence of injury on appropriate trauma CT. Any concerns regarding the need for further radiological assessment, for example MRI, should be discussed with a senior trauma clinician at MTS.
-
Receiving trauma patients in the ED

In an ED, the location for the initial assessment of trauma patients requires consideration of risks to both patients and risks to HCWs, including consideration that HCW as well as patients, may have asymptomatic COVID-19. Severely injured patients require resuscitation in appropriate settings. It is recognised that a negative pressure room is the highest level of isolation for patients:
- With unknown risk or suspected to have COVID-19.
- Requiring aerosol generating procedures (AGP).
We recommend that EDs consider the most appropriate location for managing major trauma patients.
We recommend that usual trauma reception protocols should apply with the addition of:
- Local consideration of:
- Controlled entry / exit points to the trauma resuscitation zone for staff and patients.
- Location for and minimising of PPE donning and doffing.
- Trauma team 'zero point survey' (Figure 12) including discussion on:
- PPE and wellbeing check, at 'S' self - for safety.
- Altered role allocation and wellbeing at 'T' team.
- A brief critical care resource capability update and any modifications to usual standard operating procedures at 'E' environment.
- A reiteration of limiting donning/doffing OF PPE at “P” priorities.
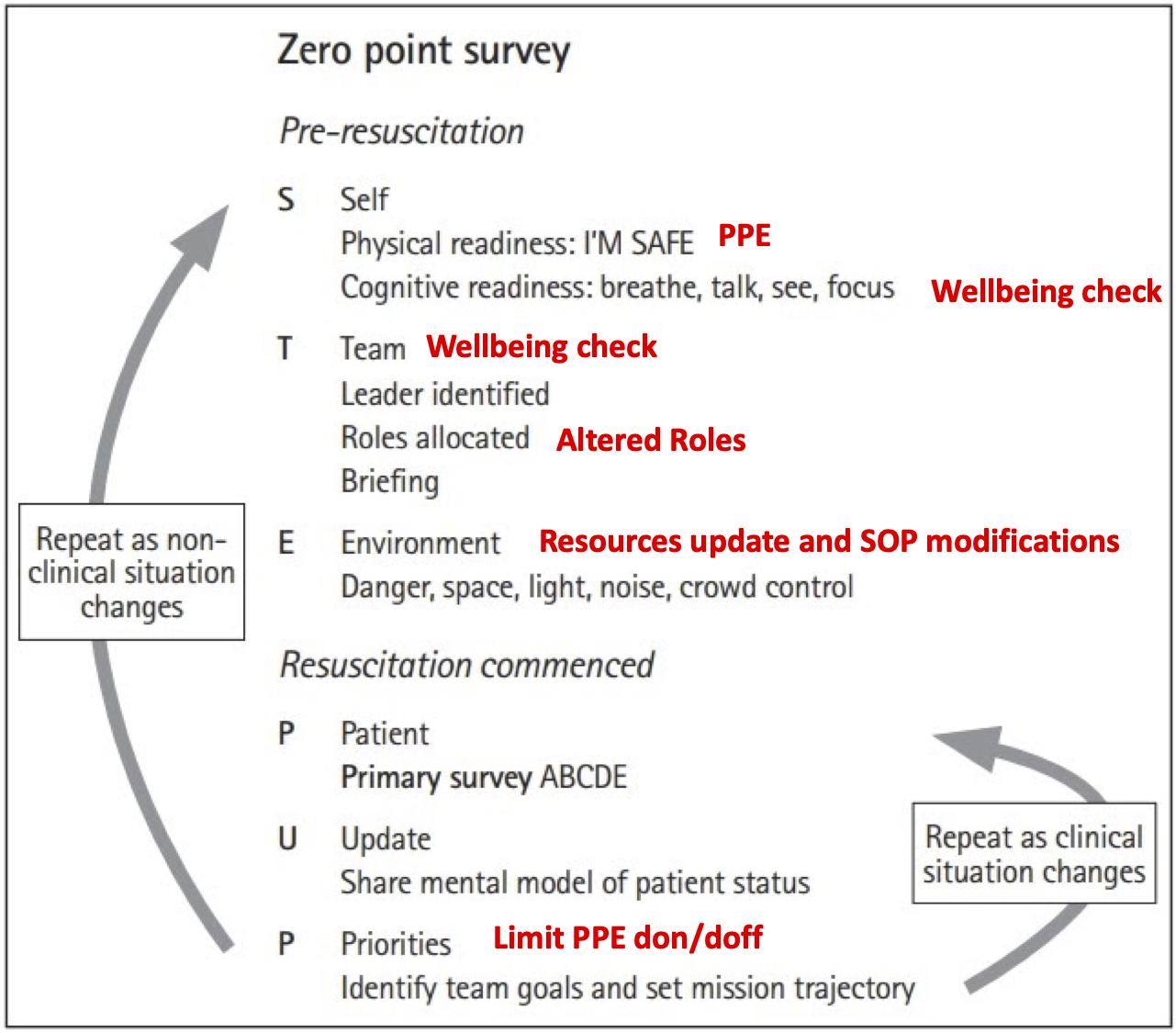
Figure 12. Zero point survey.
Adapted from Reid et al. Zero point survey: a multidisciplinary idea to STEP UP resuscitation effectiveness. [Link]
- Additional trauma team role of PPE quality assurance, which may be delegated to the existing scribe role in resource constraints.
- Traditional trauma team roles and locations are altered with:
- Use senior expertise is used to minimise the number of HCW in the trauma reception bay.
- Trauma team clinicians in the trauma reception bay wearing PPE for AGPs (Figure 13, purple).
- Trauma team clinicians outside of the trauma room wearing PPE for suspected COVID-19 patients (Figure 13, bellow).
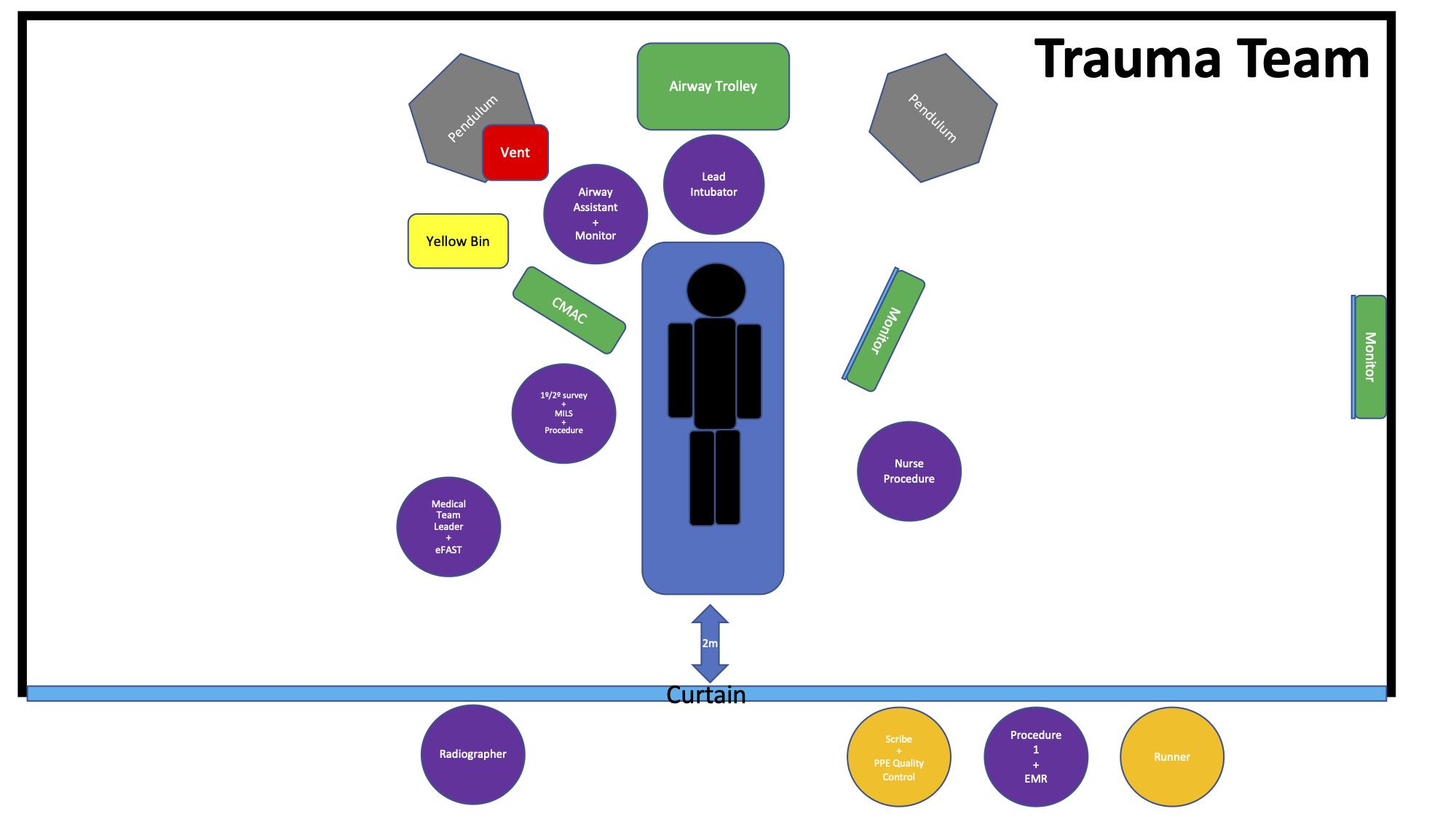
Figure 13. Trauma team roles and location.
- The trauma CT scan:
- Is minimised, where possible, when resources are overwhelmed.
- That in adult patients with moderate to severe trauma, whole body CT (WBCT) is preferred to minimise multiple selected CTs and repeated patient transport.
- Should be reviewed for both injury and incidental findings of COVID-19.
- May be deferred and augmented by plain x-ray, ultrasound and serial examination in consultation with a senior trauma clinician taking accountability for ongoing patient care.
- Is discussed with MTS for paediatric patients as CT can often be avoided.
- COVID-19 swab is considered early in line with local guidelines.
- Consideration of delayed, non-operative (e.g. interventional radiology) or conservative management for all injuries.
-
Family in the trauma room

We recommend that:
- Family is restricted from entering resuscitation rooms, except in exceptional circumstances, for example paediatric trauma, as determined by local policies.
- Social work support is provided to family members in a safe location or via telehealth where COVID-19 precludes visitation.
- Bereavement procedures follow local guidelines for COVID-19.
-
Minor trauma

Where possible, the principles of minor trauma management in COVID-19 should be to:
- Ensure essential services such as orthopaedic and plastic surgical services are maintained, while minimising impact on resources for the COVID-19 response.
- Streamline diversion of appropriate patients away from the ED.
- Consider and streamline delayed, day surgical, non-operative, or virtual solutions.
We recommend:
- Non-operative interventions were possible e.g. fracture reduction or laceration repair under local anaesthetic block.
- The use of back slabs in appropriate cases with appropriate patient information where possible, to decrease attendances for plaster removal.
We advocate for:
- Mechanisms for increased consultation to decrease unnecessary outpatient referrals.
- Specialty surgical services to provide guidance on priorities of care for example, still require admission e.g. hip fracture, non-operative care preferred e.g. some limb fractures, day case and virtual management strategies.
-
Resources

Resources that are relevant to this section can be accessed through the Clinical Guidelines web-based material [Link]. COVID-19 related ACEM Resources [Link], COVID-19 related external resources [Link], and the latest Government advice on COVID-19 [Link] are also available.
-
References

Duffy C, Kidd AC, Francis S, Tsim S, McNaughton L, Ferguson K, Ferguson J et al. Chest drain aerosol generation in COVID-19 and emission reduction using a simple anti-viral filter. medRxiv (preprint). doi: 10.1101/2020.07.13.20152264. 2020 Jul 15. [Link]
-
Section disclaimer

This section has been developed to assist clinicians with decisions about appropriate healthcare in Emergency Departments in Australia and Aotearoa New Zealand during the COVID-19 outbreak. It is a framework for planning and responding to this pandemic, including the assessment and management of patients.
This section is targeted at clinicians only. Patients, parents or other community members using it should do so in conjunction with a health professional and should not rely on the information in the guideline as professional medical advice.
The section has been developed by an expert team of practising emergency physicians, by consensus and based on the best evidence available. The recommendations contained do not indicate an exclusive course of action or standard of care. They do not replace the need for application of clinical judgment to each individual presentation, nor variations based on locality and facility type.
The section is a general document, to be considered having regard to the general circumstances to which it applies at the time of its endorsement.
It is the responsibility of the user to have express regard to the particular circumstances of each case, and the application of the section in each case.
The authors have made considerable efforts to ensure the information upon which it is based is accurate and up to date. However, the situation is rapidly evolving, and a certain amount of pragmatism needs to be employed in maintaining such a ‘living document’. Users of this section are strongly recommended where possible to confirm that the information contained within the document is correct by way of independent sources. The authors accept no responsibility for any inaccuracies, information perceived as misleading, or the success or failure of any treatment regimen detailed. The inclusion of links to external websites does not constitute an endorsement of those websites nor the information or services offered.
The section has been prepared having regard to the information available at the time of preparation and the user should therefore have regard to any information, research or other material which may have been published or become available subsequently.
Whilst we have endeavoured to ensure that professional documents are as current as possible at the time of their creation, we take no responsibility for matters arising from changed circumstances or information or material which may have become available subsequently