Depending on local epidemiology, it may be necessary for the ED to establish a ‘high-risk’ treatment zone, which separates patients with confirmed or suspected COVID-19 (as per Figure 1) from very low risk patients.
We recommend that any high-risk zone is:
- Clearly demarcated, with a minimum number of entry and exit points and designated areas for staff to don and doff PPE.
- Described using neutral language, such as a ‘hot’ or ‘red’ zone.
- Staffed by a team of dedicated clinicians separate from those looking after low-risk patients, unless the model of care allows for clinicians to safely don and doff PPE after each patient encounter.
- Assessed for adequacy of ventilation, including air flow and filtration arrangements.
- Temperature controlled to maintain staff comfort, given the PPE requirements that will apply.
We recommend that staff working in this high-risk zone:
- Wear appropriate PPE at all times (see specific recommendations in Section 6).
- Are not permitted to bring food into this or any other clinical area.
Are supported to take regular, planned breaks, as per the workforce and wellbeing section of this guideline
Design of the high-risk zone will depend on the available infrastructure, ventilation arrangements and layout of the ED. An example of a flow diagram incorporating risk assessment and zoning appears in Figure 2 below. Rapid antigen testing (RAT) may also play a role in the allocation of patients to various zones within the ED.
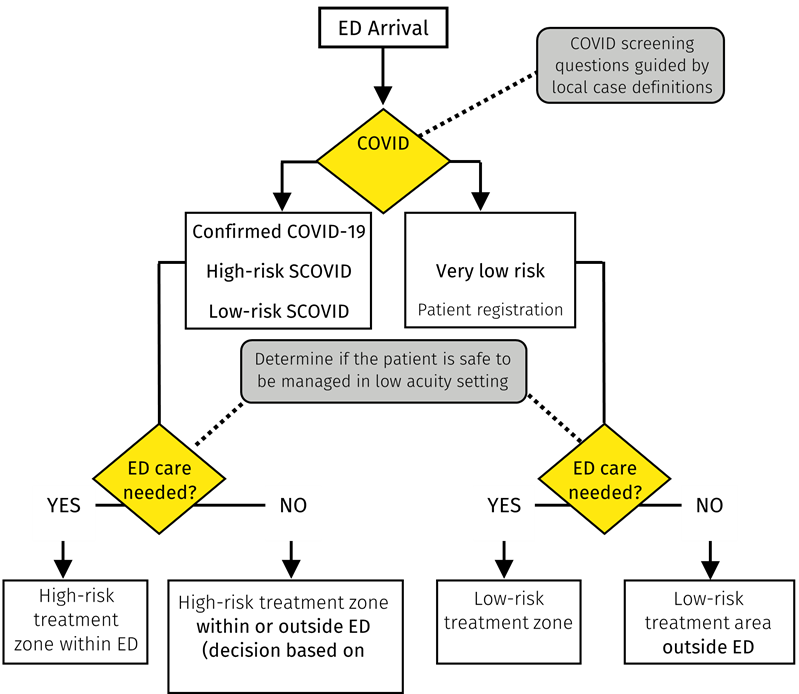
Figure 2 Example of a flow diagram incorporating risk assessment screening and zoning
In the setting of significant rates of community transmission, we recommend that consideration is given to:
- Designating the entire ED as a ‘high-risk’ zone. In effect, this would require staff to use PPE for airborne precautions for every patient interaction. This strategy may decrease the risk that staff inadvertently become ‘close contacts’ (resulting in furlough), and reduce complexity in processes.
- Implementing rapid testing procedures, such as RAT, as part of a forward triage model. This may assist with the early identification of high-risk patients, especially when history of epidemiological or symptom risk is unavailable or has become less reliable.